IBD stands for inflammatory bowel disease, which is an umbrella term used to describe disorders that cause chronic inflammation of your gastrointestinal (GI) tract. The two most common forms of IBD are Crohn’s disease and ulcerative colitis.
Path to receiving a Crohn’s disease or ulcerative colitis diagnosis can be overwhelming. Testing can be done via the following:
●Initial testing and evaluation
The first step to getting an IBD diagnosis and starting treatment involves your healthcare team obtaining a thorough medical history from you and performing a physical exam of your body.
Ensure you share with your doctor any previous medical records including summaries of visits with other doctors, lab results, and other tests that may have already been performed.
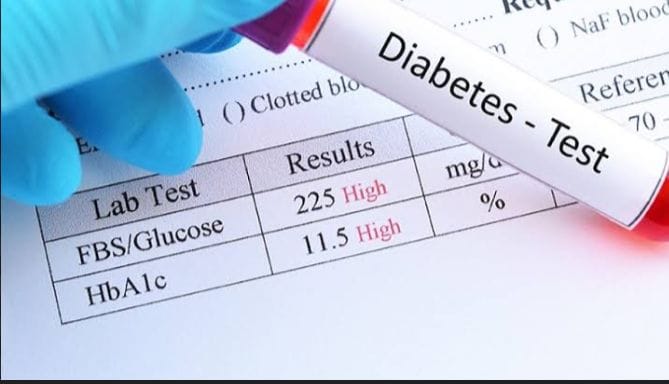
●The first tests will likely include blood and stool laboratory tests.
●Further testing could include imaging studies of the gut.
●Your doctor may also recommend a test that uses a contrast agent (oral or intravenous) that allows for a clearer and more detailed picture of your GI tract.
●Additional testing may include looking inside your GI tract using an endoscope (colonoscopy or upper GI endoscopy etc.).
● Biospy
●Radiological tests may also be done.
Learn about Crohn's disease.
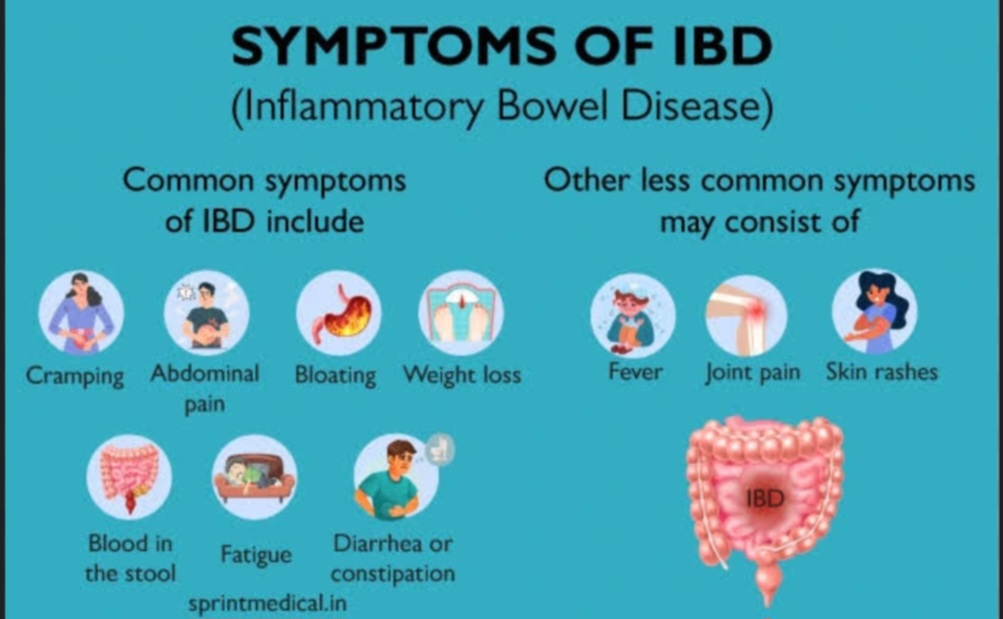
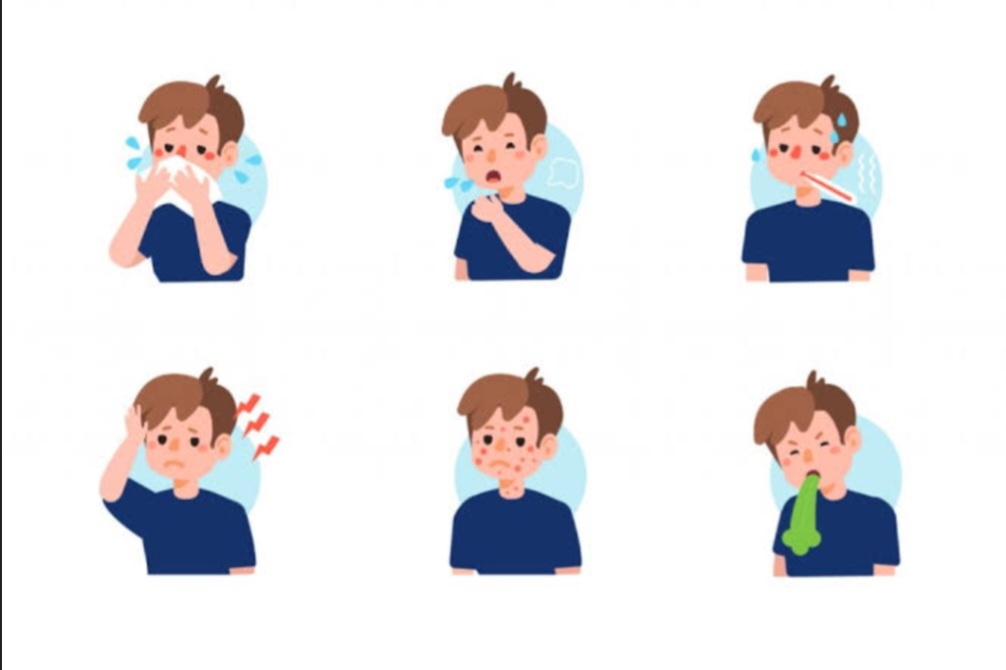
While it is important to recognize the signs of Crohn’s disease, only a doctor can confirm a diagnosis. The common symptoms can be grouped as follows:
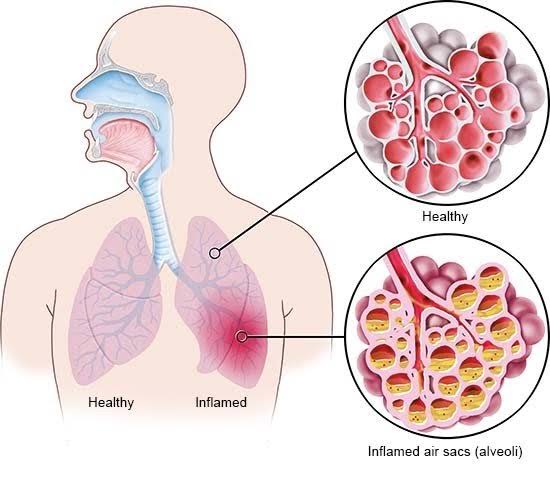
- GI Tract Inflammation
Crohn’s disease can affect any part of the GI tract, from your mouth to your anus. Symptoms vary from patient to patient. Some common symptoms of inflammation include:
•Persistent diarrhea
•Rectal bleeding
•Urgent need to move bowels
•Abdominal cramps and pain
•Sensation of incomplete bowel evacuation
•Constipation, which can lead to bowel obstruction
- Crohn’s Disease Complications
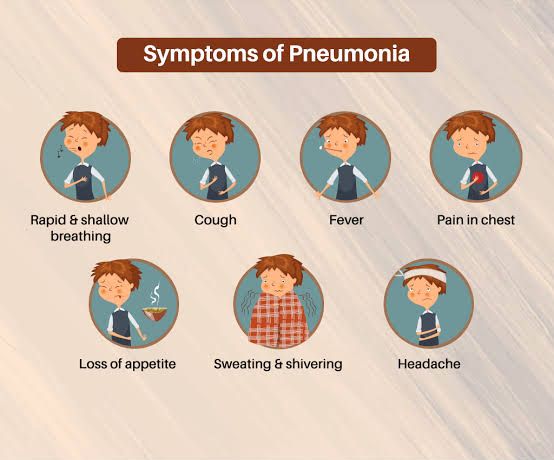
•Loss of appetite
•Weight loss
•Low energy and fatigue
•Delayed growth and development in children
In more severe cases, serious complications arise such as:
•Fissures are tears in the lining of the anus, which can cause pain and bleeding.
•Formation of a fistula—an abnormal channel between the intestine and the anal canal, bladder, vagina, skin, or another part of the intestine. Fistulas are most common in the anal area.
•A stricture -narrowing of the intestine as a result of chronic inflammation.
- Systemic complications
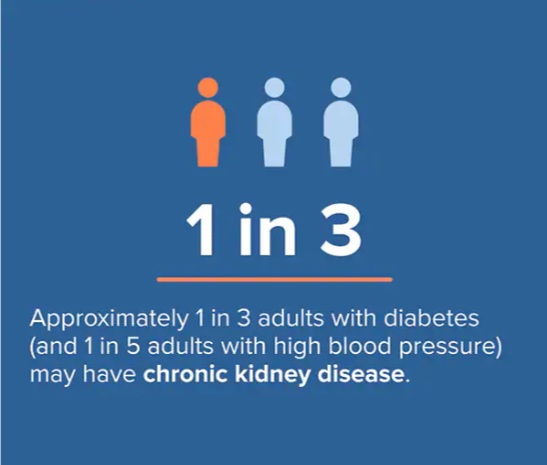
•Inflammatory bowel disease (IBD) can cause systemic symptoms outside the GI tract i.e in the kidney, eyes, joints, skin, hormonal changes, and some rare liver complications.
N/B: Crohn's disease is more common between ages 15 to 35.
It is majorly genetic in nature.
Learn about Ulcerative Collitis
Ulcerative colitis is a chronic disease of the large intestine, in which the lining of the colon becomes inflamed and develops tiny open sores, or ulcers. This condition is the result of your immune system’s overactive response.
If you experience any of these symptoms, consult your healthcare provider.
•Loose and urgent bowel movement
•Bloody stool
•Abdominal cramps and pain
•Persistent diarrhea accompanied by abdominal pain and blood in the stool
N/B: Your ulcerative colitis symptoms will come and go, with longer periods in between flares when you may not experience any discomfort at all (remission) and they can span months or even years.
Other symptoms include:
•Loss of appetite
•Weight loss
•Nausea
•Fever
•Low energy and fatigue
•Anemia (low red blood cell count)
•Delayed growth and development in children