Malaria remains a significant health concern in Kenya and other tropical regions. Effective prevention and awareness are crucial in reducing its impact.
What is Malaria?
Malaria is a serious disease caused by Plasmodium parasites, transmitted through the bite of infected Anopheles mosquitoes. It’s common in tropical and subtropical regions, including many parts of Africa.
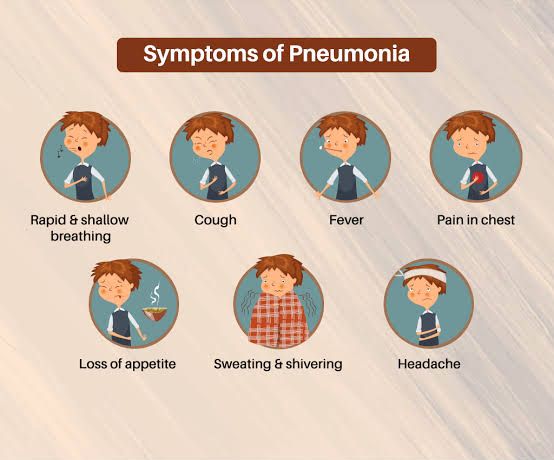
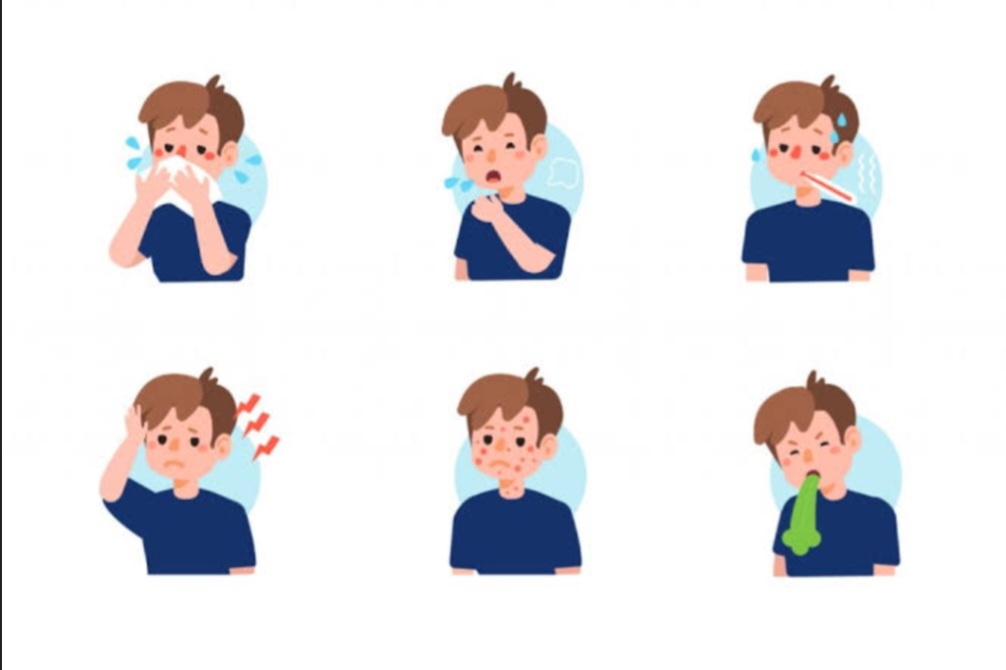
Signs and Symptoms of Malaria
Symptoms usually appear 10–15 days after a mosquito bite. If untreated, malaria can become severe and even life-threatening.
Note: Symptoms are usually dependent on the plasmodium strain.
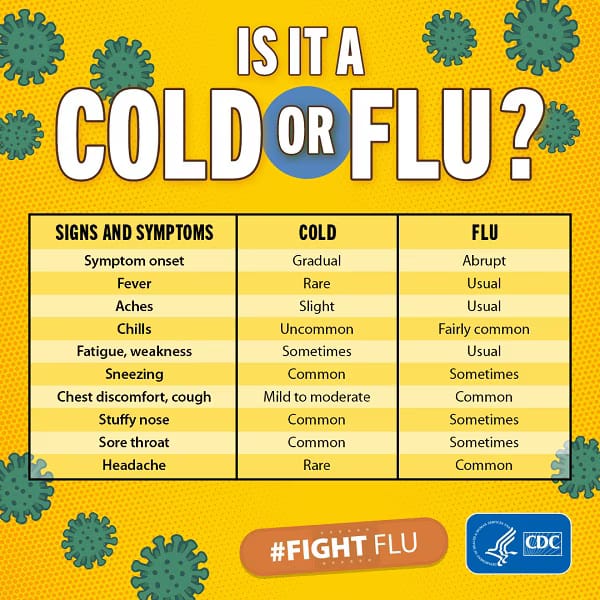
Common Symptoms
- Fever and chills
- Sweating
- Headache
- Nausea and vomiting
- Muscle aches
- Fatigue or weakness
- Rapid breathing
- Cough (in some cases)
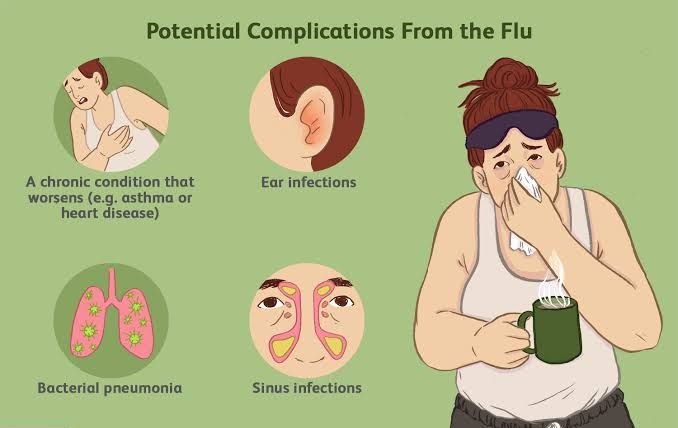
Severe Symptoms (Seek emergency care)
- Seizures
- Confusion
- Loss of consciousness
- Severe anemia
- Kidney failure
- Difficulty breathing
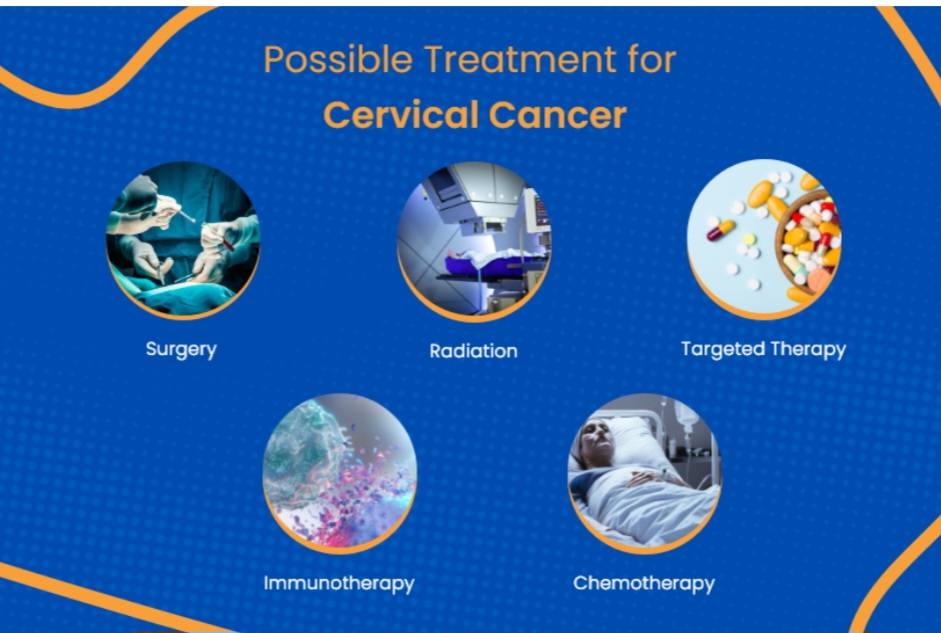
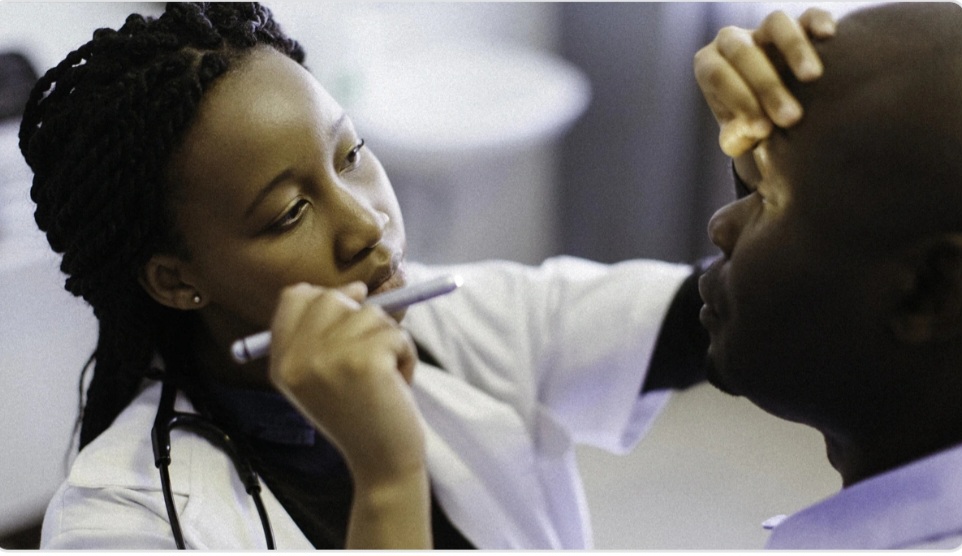
Malaria Treatment
Malaria is treatable if diagnosed early. Treatment depends on:
- The type of Plasmodium
- Severity of symptoms
- Patient age and health condition
First-line Treatments:
Artemisinin-based combination therapy (ACT): Most effective for P. falciparum.
Chloroquine: For P. vivax, P. ovale, and P. malariae (where not resistant).
Primaquine: Used to eliminate dormant liver stages of P. vivax and P. ovale to prevent relapse.
Important Treatment Tips include:
- Completing the full course of medication.
- Avoiding self-medication
- Proper care for Pregnant women, children, and individuals with weak immunity.
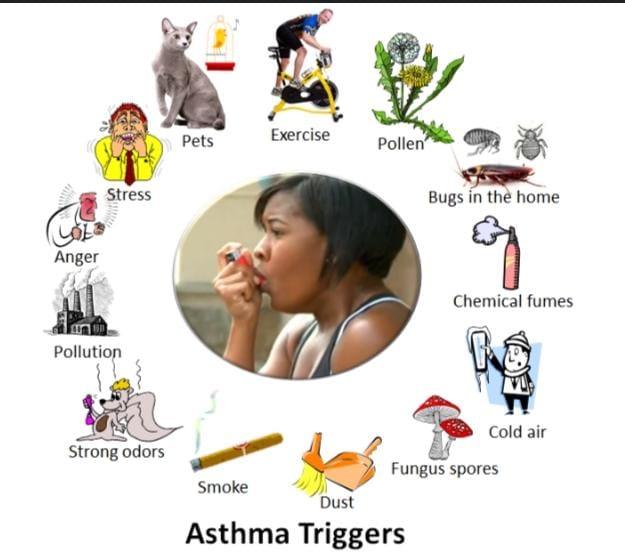
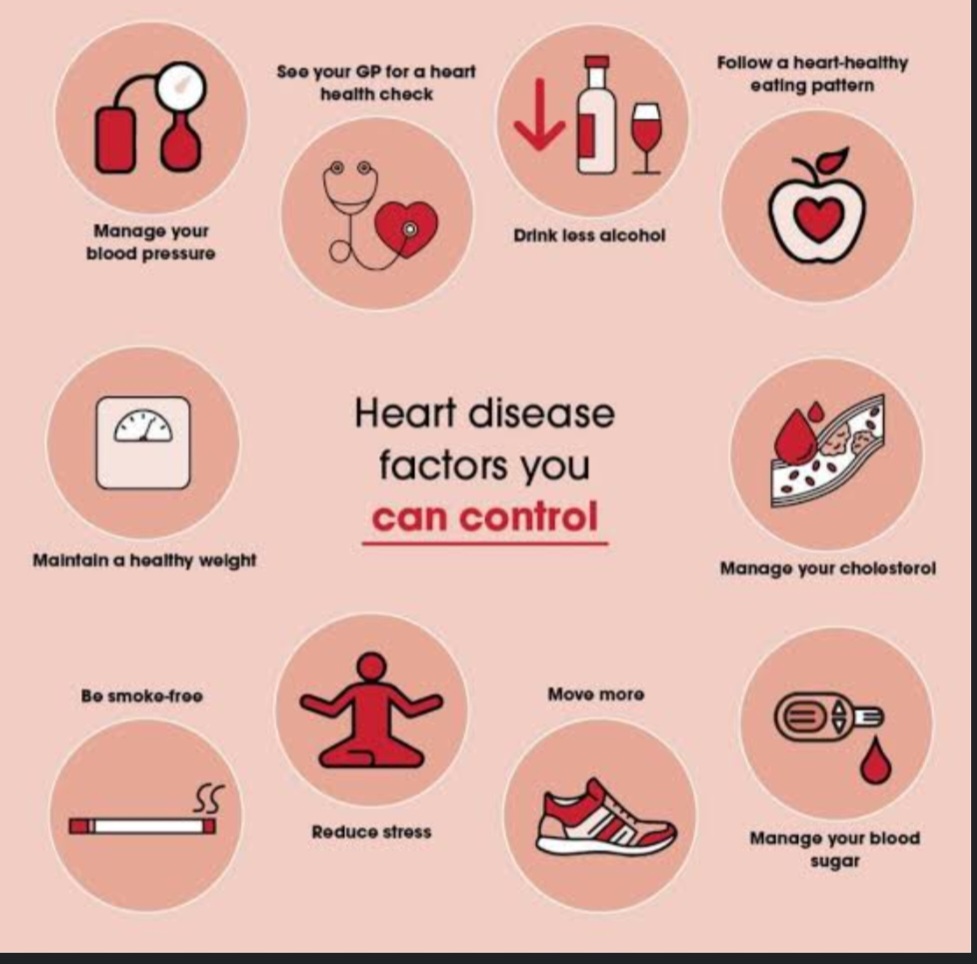
Tips for Prevention
- Avoid mosquito bites by use of insecticide-treated mosquito nets or applying mosquito repellent.
- Beware of the malaria endemic regions and ensure you take preventive medication when traveling to malaria-risk zones.
- Ensure your environment does not promote mosquito breeding i.e Eliminate standing water near your home.
- Seek medical help immediately if you notice symptoms after visiting a malaria-prone area.
- Chemoprophylaxis (Preventive Medication): Consult Healthcare Providers before traveling to malaria-endemic areas, seek medical advice on suitable antimalarial medications. Common Antimalarial Drugs include: Atovaquone-Proguanil (Malarone), Doxycycline and Mefloquine. Consult your health provider on how and when to take these medicines.
- The WHO recommends RTS,S/AS01 (Mosquirix) vaccine for children in malaria-endemic regions to prevent Plasmodium falciparum malaria. Consult Local Health Authorities for vaccination availability and eligibility.
New Strains & Drug Resistance
Some malaria strains now carry multiple Plasmodium species, such as both P. falciparum and P. vivax.
This leads to Mixed Infections in many malaria-endemic regions complicating diagnosis and treatment.
N/B: The Anopheles stephensi vector originally native to South Asia, has been detected in parts of Africa and is capable of transmitting both P. falciparum and P. vivax, increasing the risk of malaria outbreaks in urban settings such as Nairobi that were originally considered malaria safe zones
Drug-resistant malaria is emerging in parts of Africa and Asia. This is caused by Plasmodium falciparum Mutations: Recent studies have identified mutations in P. falciparum that confer resistance to multiple first-line antimalarial drugs, especially artemisinin.
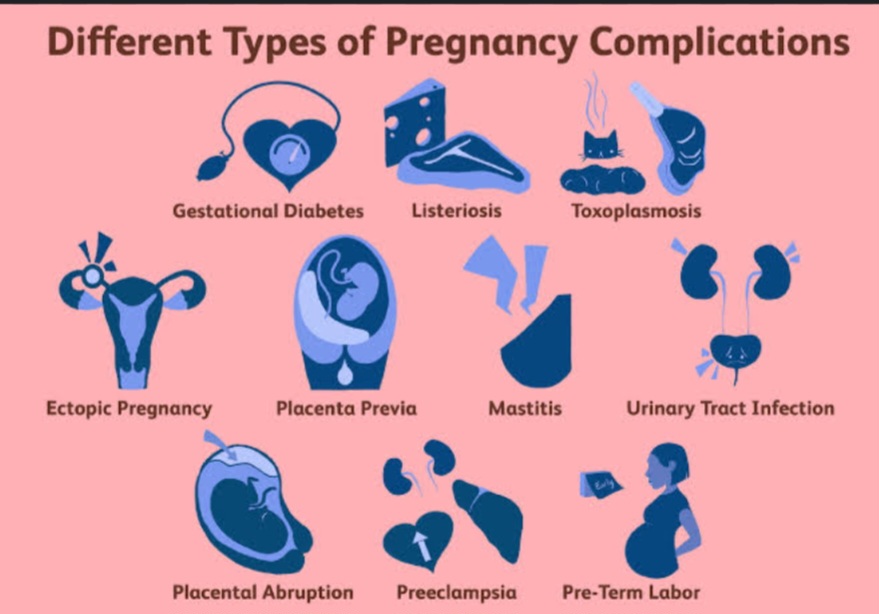
Malaria and Pregnancy
Special Care should be accorded to Expecting Mother especially in the first trimester due to changes in immunity.
Malaria during pregnancy can lead to: Severe anemia, Miscarriage or stillbirth, Low birth weight, Premature delivery or Maternal death.
Prevention Tips for Pregnant Women:
- Use Insecticide-Treated Nets (ITNs)
- Take Intermittent Preventive Treatment (IPTp): In malaria-endemic regions, WHO recommends Sulfadoxine-Pyrimethamine (SP) starting from the second trimester, taken at least 3 times during pregnancy.
- Attend All Antenatal Visits: Ensures timely malaria testing and preventive treatment.
- Seek Immediate Medical Attention if you develop fever, chills, or other symptoms.
Key notes:
In Kenya the following areas are categorized as Malaria Endemic Zones (High Risk All Year Round)
Counties:Kisumu, Siaya, Homa Bay, Migori, Busia, Kakamega, Bungoma, Vihiga, Parts of Kisii and Nyamira ( Western Kenya and Lake Victoria basin, where warm, humid climate supports mosquito breeding year-round)
Seasonal Transmission Zones (Moderate Risk) include :
Counties: Baringo, Elgeyo Marakwet, West Pokot, Parts of Narok and Samburu (Malaria cases rise during and after the rainy season due to favorable breeding conditions)
Epidemic-Prone Areas
Counties: Kericho, Nandi, Uasin Gishu, Trans Nzoia, Laikipia, Nyandarua, Parts of Meru and Embu.( Usually low risk, but have outbreaks during climate changes. Stay vigilant to know about such outbreaks.
Low Risk or Malaria-Free Zones
Counties: Nairobi, Nyeri, Kiambu, Murang'a, Nyahururu, Machakos (urban zones)
Note: Risk is very low but not zero. However the Anopheles stephensi vector threatens to change this status in urban areas.